MACRA and NCQA Recognition Programs
MACRA rewards clinicians who earn NCQA Patient-Centered Medical Homes (PCMH) and Patient-Centered Specialty Practices (PCSP) Recognition.
The Medicare Access and CHIP Reauthorization Act (MACRA) is a payment program from the Centers for Medicare & Medicaid Services (CMS). MACRA replaced the Sustainable Growth Rate (SGR) formula for how CMS pays clinicians caring for Medicare beneficiaries. It makes patient-centered care the key to success for clinicians.
MACRA rewards clinicians who earn NCQA Patient-Centered Medical Homes (PCMH) and Patient-Centered Specialty Practices (PCSP) Recognition.
How Does MACRA Impact Clinician Payment?
Beginning in 2019, clinicians will receive payments through either the new Merit-Based Incentive Payment System (MIPS) or Alternative Payment Models (APMs). Most clinicians will receive payments through MIPS. The 2019 payment will be based on what clinicians did and reported in 2017.
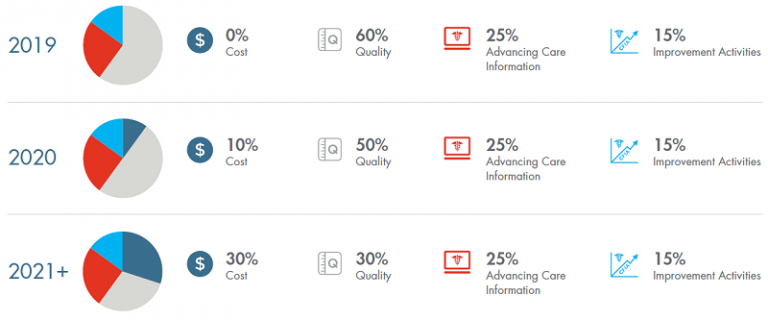
Clinicians in MIPS will get bonuses (or penalties) to their fee-for-service payments based on measures in four areas. The proportions of the four areas that make up MIPS scores scale up until 2021, when they become permanent:
MIPS Payments and NCQA Recognition
Becoming an NCQA Recognized PCMH/PCSP directly increases clinicians’ payments through MIPS. Clinicians in these PCMHs/PCSPs automatically get full credit in the MIPS CPIA category and will likely do well in other MIPS categories.
- Quality Measures: PCMHs/PCSPs increase the use of high-value care. This includes prevention and good chronic care management, promoting quality improvement that will be reflected in MIPS quality measures.
- Advancing Care Information: Recognition emphasizes coordination of care and the use of HIT to share care information.
- Resource Use Measures: Evidence shows that the PCMH model is saving money by reducing hospital and ED visits and improving patient outcomes.
Alternative Payment Models
Alternative Payment Models move clinicians away from fee-for-service toward quality and population-based payments. Clinicians who meet specific dollar and patient volume thresholds, qualify as “Advanced APMs”. They are exempt from MIPS and eligible for automatic 5 percent bonuses on their Medicare payments. For clinicians in APMs that do not meet the thresholds, the proposed MACRA rule rewards clinicians in APMs with NCQA-Recognized PCMH/PCSP.
More PCMH/PCSP Clinicians Means Higher MIPS Scores
How the scoring works:
- Clinicians in APMs are scored individually. CMS averages scores for all clinicians in the APM and applies the average score to each clinician.
- Clinicians in PCMHs/PCSPs get automatic full CPIA credit. Clinicians who have not earned recognition get half CPIA credit for being in the APM and must earn additional CPIA points for individual CPIA activities.
- Having more PCMH/PCSP clinicians in an APM automatically gives all of that APMs’ clinicians higher MIPS scores.
Free MACRA Toolkit
Want to learn more about how to implement a patient-centered approach to help achieve your MACRA goals? Visit macratoolkit.com for a free toolkit.
- Save
Save your favorite pages and receive notifications whenever they’re updated.
You will be prompted to log in to your NCQA account.
Save your favorite pages and receive notifications whenever they’re updated.
You will be prompted to log in to your NCQA account.
- Email
Share this page with a friend or colleague by Email.
We do not share your information with third parties.
Share this page with a friend or colleague by Email.
We do not share your information with third parties.
- Print
Print this page.
Print this page.
- Current Customer? Ask a Question
Using My NCQA
- Interested in PCMH? Contact Us Today!
We're Here To Help.