Person-Centered Outcome Measures
Quality Measures for What Matters Most.
Everyone deserves fair and just access to high-quality health care that addresses their unique needs and is designed to deliver the outcomes they want.
Everyone deserves fair and just access to high-quality health care that addresses their unique needs and is designed to deliver the outcomes they want. This is particularly true for people with complex health care needs, many of whom are older adults who often receive care that may be misaligned with their needs and goals. Nearly 30% of Medicare beneficiaries have complex health care needs, and more than 14 million people in the U.S. need long-term services and supports. These numbers are growing every year.1
Measuring What Matters
What are the PCO measures?
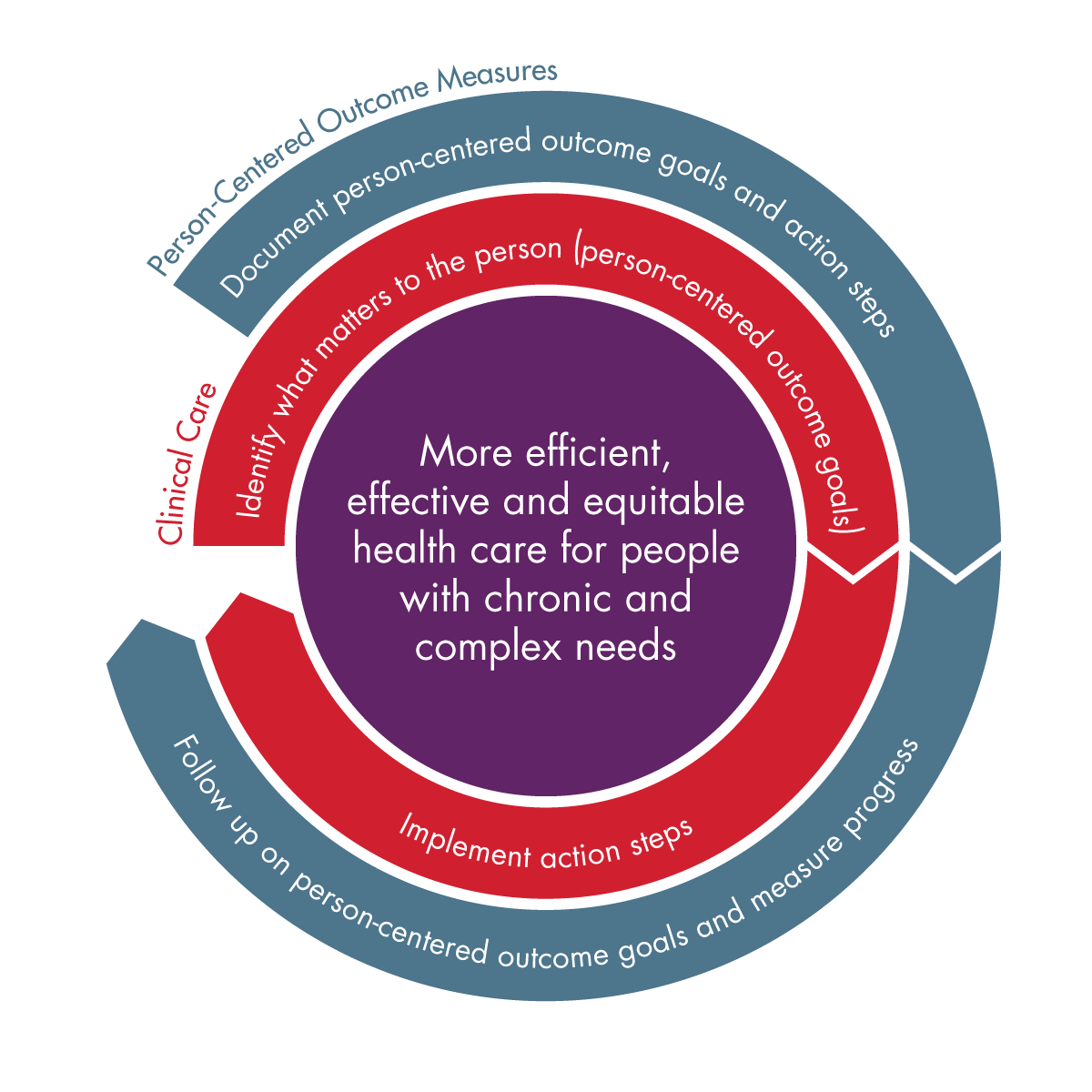
Person-Centered Outcome (PCO) measures work in tandem with clinical care to help people living with complex health needs make progress toward a person-centered outcome goal that matters to them. Clinicians throughout the care continuum and community-based services can use this approach to identify what is important to a person.
After capturing what matters, the clinician documents these person-centered outcome goals and collaborates with the person on action steps to achieve them. The PCO measures standardize documentation and tracking, and measure progress using patient-reported outcome measures (PROMs) or goal attainment scaling (GAS). Within six months, the clinician completes a follow-up visit with the individual, in-person or telephonically, to assess progress on the person-centered outcome goal. This approach breaks down into three measures:

Goal Indentification:
Percentage of individuals 18 years of age and older with a complex care need who had a PCO goal identified, resulting in completion of GAS or a PROM and development of an action plan.

Goal Follow-Up:
Percentage of individuals 18 years of age and older with a complex care need who received follow-up on their PCO goal within two weeks to six months of when the goal and GAS or PROM were identified.

Goal Achievement:
Percentage of individuals 18 years of age and older with a complex care need who achieved their PCO goal within two weeks to six months of when the goal and GAS or PROM were identified.
How are PCO measures different from traditional quality measures?
Unlike traditional measures that are checkbox, disease focused or exclude older adults from the denominator, the PCO measures incorporate the individual's voice into the care plan and quality measurement. These measures are applicable for all individuals 18 years of age or older with a complex care need.

The video below demonstrates the real-world impact of person-centered care and how quality measures like, the PCO measures, can be used to assess the quality of care provided.
Using PCO Measures
Where have the PCO measures been implemented?
To date, the NCQA PCO measures have been successfully tested in multiple care delivery settings in over 30 practices, with more than 300 clinicians (e.g., physicians, nurses, social workers, peer navigators, and care managers) and 9,800 individuals.
Primary Care
- Home-Based Primary Care
- Serious Illness Programs
- Care Management
Long-Term Services and Supports (LTSS)
- Area Agencies on Aging
- Community-Based Organizations
Behavioral Health
- Certified Community Behavioral Health Clinics (CCBHCs)
- Behavioral Health Homes
Health Plans
- Special Needs Plans (SNPs)
What have we learned from implementation efforts? PCO Measures Deliver High-Quality Care!
Findings from testing show that individuals, care partners and clinicians found value in setting personalized measurable goals in care visits and that the person-centered outcome approach was feasible. Many individuals stated they had never been asked what mattered most to them and had a clinician follow-up on that goal. It helped build trust early in the patient/clinician relationship and provide an opportunity to tailor the care plan appropriately.
Other benefits include:
| Benefits of PCO Measures | |
|---|---|
| For People |
|
| For Clinicians |
|
| For States and Health Plans |
|
"The whole point of my goal was to be able to get out and be more physically active, to the point where it doesn't feel like a chore anymore.
I'm not struggling to get out and be functional. And it's amazing. Because going from not being able to do anything at all, to slowly starting to feel like my old self again, is kind of a miracle. I was able to play with my nieces and I was actually able to keep up. I feel better."
Increasing Adoption
In order to increase widespread adoption of the PCO measures, we need the help of many stakeholder groups, including:
Clinicians:
Current measures are checkbox and disease-focused and do not incorporate the individuals needs into the care plan. Clinicians have stated these measures are more meaningful and preferred to existing measures.
Consumer Advocates:
Consumer Advocates are dedicated to improving patient outcomes and aligning care with an individuals needs. The PCO measures incorporate what matters most into care planning and quality measurement. This type of approach needs to be advocated for across the entire health journey to deliver person-centered care at the highest value and lowest cost.
Special Needs Plans (SNPs):
CMS requires SNPs to have and implement a Model of Care, which is a basic framework to provide the highest quality of care for enrollees and requires SNPs to document and collect goals. However, there is no standardized approach for documenting and tracking a goal conversation. Building the PCO approach into existing clinical workflows can support these goal conversations.
State Medicaid:
Many existing State program requirements include goal conversations but there is no structure around the conversation or payment incentives. Adding PCO measures into existing or new State program requirements for value-based payment or quality improvement purposes can support person-centered care into clinical workflows.
Take the Next Step
Consumer Advocacy
Share the PCO Approach toolkit to help your members implement the PCO approach.
Educate your constituents on the impact of the PCO measures and how they can improve care.
Clinicians
To learn how to implement the PCO approach, take our free, online trainings or review our PCO approach toolkit:
- Identifying and Developing a Person-Centered Outcome Goal (Behavioral Health Version)
- Using Goal Attainment Scaling to Document and Track Person-Centered Outcome Goals (Behavioral Health Version)
- Using Patient-Reported Outcome Measures to Document and Track Person-Centered Outcome Goals (Behavioral Health Version)
Learn first-hand the value of these measures for individuals:
Special Needs Plans (SNPs)
- CMS requires SNPs to implement a Model of Care. The PCO measures can provide the structure to that process.
- PCO measures are on the path to becoming HEDIS measures. Becoming an early adopter can make sure you are ready for when they are required for reporting.
Contact the PCO measures team to join the SNP Learning Collaborative to get support to implement the PCO measures at your plan.
State Medicaid
Check out these resources to learn more about how these measures can benefit state programs:
"I knew that it was going to be a success, because in health care sometimes we’re so busy that we forget to stop and ask people what they actually want."
Social Worker"[For] patients, getting to the heart of, 'Is it the care that they actually want to receive?' helps them be more engaged and also makes them happier."
Site AdminstratorAdditional Resources
PCO Approach Trainings
- Identifying and Developing a Person-Centered Outcome Goal (Behavioral Health Version)
- Using Goal Attainment Scaling to Document and Track Person-Centered Outcome Goals (Behavioral Health Version)
- Using Patient-Reported Outcome Measures to Document and Track Person-Centered Outcome Goals (Behavioral Health Version)
Companion Resources to Trainings
Publications
- Refining a Taxonomy of Goals for Older Adults With Functional Limitations and Their Caregivers to Inform Care Planning
- Standardized approach to measuring goal-based outcomes among older disabled adults: results from a multisite pilot
- Patient and provider perspectives on using goal attainment scaling in care planning for older adults with complex needs
Webinars
- Person-Centered Outcome Measures: Measuring What Matters Most
- Person-Centered Outcomes: A New Approach for Delivering Quality Care
- NCQA 2022 Health Innovation Summit Session: Promoting Equity by Measuring What Matters Most
- NCQA 2023 Health Innovation Summit Session: Incorporating What Matters into Measurement and Person-Centered Care
Blogs
Allies & Partners
We are grateful to our many colleagues and collaborators that share NCQA's commitment to health equity.
Contributions and contributors shaping development of measures and practices related to person-centered care:
- Patient Priorities Care (Patient-Facing Platform: My Health Priorities)
- Age-Friendly Health Systems
- Alliance for Person-Centered Care
- Camden Coalition's The Blueprint for Complex Care
- Center for Health Care Strategies
We also thank the funders that make it possible for us to develop measures to support individuals with complex care needs:
