December 22, 2020
Brett Giroir, M.D.
Assistant Secretary for Health
Department of Health and Human Services
200 Independence Ave. S.W.
OASHcomments@hhs.gov
Dear Assistant Secretary Giroir:
The National Committee for Quality Assurance (NCQA) is pleased to respond to your Request for Information (RFI) on how to leverage novel technologies for chronic disease management in aging underserved populations. Novel technologies like artificial intelligence (AI), biosensors, apps and remote monitoring have enormous potential to improve care for all patients, but especially chronic disease management in older, underserved Americans. NCQA is working to promote and accelerate development of the Digital Quality Ecosystem (DQE) through public and private partnerships to facilitate a wide range of clinical insight sharing and quality improvement, management, and value-based incentive programs. Like novel technologies, this holds great promise for improving care management for all patients and especially older, underserved Americans.
Background. For the last 30 years quality measurement has driven remarkable improvements in healthcare. The Healthcare Effectiveness Data and Information Set (HEDIS©), the backbone of the measurement system, has revolutionized our ability to identify areas for improvement, drive that improvement and standardize expectations for high quality care. Adoption of HEDIS measures aimed at the prevention and treatment of colorectal cancer, high blood pressure and diabetes, to name a few, have resulted in millions of saved lives and avoided complications.
Problem. Today’s sprawling quality enterprise can be labor-intensive, fragmented and inconsistent. It is also largely retrospective. Eliminating unnecessary or duplicative work and expenditures related to quality measurement could result in massive cost savings and free up invaluable time for patient care. America needs a more automated, unified, accurate, prospective, and timely quality measurement and reporting system. Moreover, the federal government bases many of its performance incentives on insufficiently validated data processed through systems that are prone to error. This undermines CMS’s goal of rewarding high quality care and ensuring that this is what patients receive.
While programs that utilize and audit HEDIS data, such as Medicare Advantage Stars, can be confident in the validity of the data used to evaluate quality, others have inconsistent – or nonexistent – validation regimes. The explosion in electronic clinical data with the adoption of EHRs makes it all the more essential that CMS evolve technology-enabled approaches to validate and leverage clinical data sources for use in quality and incentive programs.
Challenges: The current approach to quality improvement and value-based incentives is fragmented and uncoordinated. This creates excessive burden on providers and hinders patient safety, efficacy, and affordability. This “non-system” produces care riddled with gaps, redundancies, and inefficiencies. Even physicians who attempt to coordinate and rationalize care are obstructed by the balkanization of data, lack of a full picture of what is happening to their patients, and inability to act effectively if care is not what it should be.
Quality is the first business use case for clinical data that we digitized over the past decade and for which digital quality can help realize its full value. Quality improvement is a top priority for patient-centered care, impacts core financial incentives in rapidly growing value-based programs (VBP), and helps remove vast amounts of waste from the system. DQE can help to achieve a future in which we make quality data more valid, trustworthy and meaningful for VBP.
The digital future that NCQA envisions would support digital quality measurement (dQM), clinical guidelines and associated decision support, electronic data collection, validation, and reporting, and other crucial functions to enable a learning measurement system. Specifically related to chronic disease, many past efforts have struggled because of care delivery paradigms and incentives built around the office or hospital “visit.” The promise of the DQE is a more connected system of clinical insights, enabling care plans and interventions to follow patients when and how they engage with their health, including via virtual care/ telehealth. The DQE would provide a substantial and urgently needed overhaul of today’s labor-intensive, fragmented, inconsistent, and retrospective quality enterprise. It aligns closely with the “secure, data-driven ecosystem to accelerate research and innovation” contemplated in the 2020–2025 Federal Health IT Strategic Plan. It is the best way to support the Centers for Medicare & Medicaid Services (CMS) goal of having all-digital quality reporting by 2030. And it aligns with growing interest among states and many private payers to move in this direction. Perhaps most importantly, a robust and digitally streamlined clinical quality infrastructure addresses the core barrier to value-based payment adoption: trusted, transparent, comparable, and timely insight into quality of care.
The DQE would facilitate specific goals cited in your RFI, such as advancing data availability from health systems (claims, electronic health records (EHR), surveillance data, etc.), applying AI to inform behavior change through remote monitoring, and assessing risk to apply appropriate preventive and acute care.
This can lead to development of projects looking at how technology can optimally interface with chronic care management at a person-specific level. For example, each individual patient has various things they could or should do for their health depending on their specific comorbidities. Individual patients also have their own unique sets of social determinants that require tailored approaches. Technology in the DQE enables chronic care management programs to support the individual patient in a way that appreciates how each of these variables are interrelated (clinical practice guidelines and care pathways). From there we can develop an ideal care scenario for each person that incorporates their own personal goals, and develop models using home monitoring and phone apps that track status on blood sugar and pressure, diet, exercise, weight, mood etc. in real time.
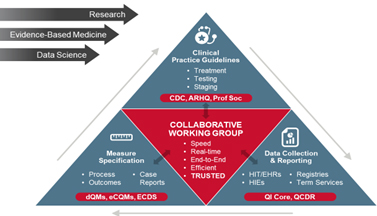 In the DQE, quality measures can flow from care that is assisted by digital clinical practice guidelines and decision supports in a continuous, near-real-time feedback loop. This is the learning measurement system referenced above. This will be a substantial improvement over the slow, linear approach for developing these crucial quality improvement tools today. This builds on work underway at the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, the Office of the National Coordinator for Health IT and others.
In the DQE, quality measures can flow from care that is assisted by digital clinical practice guidelines and decision supports in a continuous, near-real-time feedback loop. This is the learning measurement system referenced above. This will be a substantial improvement over the slow, linear approach for developing these crucial quality improvement tools today. This builds on work underway at the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, the Office of the National Coordinator for Health IT and others.
The DQE can continuously evolve and expand to incorporate new users, use cases and functionalities. For example, NCQA has already launched a Digital Measurement Community, established to foster collaboration and consensus processes for broad adoption of digital quality tools and approaches.
Barriers: A key barrier to realizing the benefits of digital quality to improve chronic disease management in underserved older adults is overcoming inertia and developing coordination among diverse stakeholders to build, test and implement the infrastructure. Demonstrating the DQE’s capacity to redirect resources required for low-value work in today’s inefficient system into higher-value, more differentiating, patient and customer-focused uses, such as improving chronic disease management for underserved older adults, can help with this.
Federal quality initiatives and policies that currently operate largely independently limit the capacity to deploy and scale technology-driven solutions for aging populations. The DQE can play a pivotal role in bringing these initiatives together in a cohesive manner that also can be coordinated with state and private payers to dramatically reduce the burden and increase the value of these programs for providers and patients. Providing federal support as part of a public-private partnership to help launch and refine the DQE could facilitate the success of technology-driven solutions for aging populations and others.
Data integrity issues are another challenge, especially for older adults in fee-for-service payment programs in which it is difficult to audit and validate data from multiple independent practices from which older underserved adults receive care. NCQA recently completed a Data Aggregator Validation (DAV) pilot demonstrating that we can validate data ingested from multiple practices by health information exchanges (HIE) or other data “hubs,” and we have launched an “early adopters” DAV program that will evolve the data quality and validation facets of the future DQE. Requiring this level of rigorous data validation across all programs serving older underserved adults can help ensure accurate and reliable quality data that we need for optimal care and VBP.
There are interoperability and standardization challenges that 21st Century Cures Act regulations and the consensus emerging from HL7 International and others help to address. But there remains persistent variation in implementations of standards that prevent practical interoperation among stakeholders. Digital quality is an ideal business case to drive adoption of the interoperability and standardization policies to meet business needs that are both tied to incentives and required for most entities. Demonstrating to regulators, developers and users of quality measures how common approaches and infrastructure can facilitate broadly shared goals opens the door to many more high-value clinical use cases.
There further are significant gaps in access to broadband, technology, and digital literacy, particularly for underserved populations. We must promptly expand Federal efforts to address the lack of broadband and these other gaps that increasingly contribute to disparities as health care moves into the digital age.
Thank you again for the opportunity to share our thoughts on this priority. We would be happy to meet with you to further detail our vision for the DQE and optimal chronic care management described above. To schedule such a meeting, or for any other questions, please contact Paul Cotton, Director of Federal Affairs, at (202) 955-5162 or cotton@ncqa.org.
Sincerely,
Margaret E. O’Kane
President
