August 31, 2020
Lance Robertson
Assistant Secretary for Aging
Administrator, ACL
Re: ACL Strategic Framework for Action: State Opportunities to Integrate Services and Improve Outcomes for Older Adults and People with Disabilities
Assistant Secretary Robertson:
The National Committee for Quality Assurance (NCQA) appreciates the opportunity to provide feedback on the ACL Strategic Framework for Action: State Opportunities to Integrate Services and Improve Outcomes for Older Adults and People with Disabilities.
States and CBOs (community-based organizations) heard Assistant Secretary Lance Robertson’s 2019 message of evolving and transforming to meet the times, and many are using NCQA Accreditation to drive person-centered quality. CBOs are evolving from “Blockbuster video” models to “Netflix streaming” and are innovating forward to the future of a digital age, with the understanding that the needs of beneficiaries remain complex, funding streams have diversified and strong relationships with delivery system stakeholders must be woven into the care continuum.
The COVID-19 pandemic has hurried states and CBOs to navigate LTSS remotely and creatively, including through increased use of telehealth vs. in-person doctor visits. The immediacy of the public health response underscores how important it is for CBOs to be prepared to meet expanding expectations and needs.
We strongly support ACL and the roadmap for CBOs, states and payers to increase interconnectivity and provide quality care that responds to the unique needs of aging persons and persons with disabilities. Below are our comments of support and our recommendations.
Section 1: Opportunities for Aging and Disability Networks
Governance and Administration
NCQA supports ACL’s guidance to states for establishing a uniform set of guidelines and expectations about roles and responsibilities and for using a strategy of collaborative governance and administration to maximize and strengthen the infrastructure of aging and disability networks. State Medicaid programs can create a plan to drive collaboration and demonstrate a united vision for quality through the state Medicaid Quality Strategy.
States are leveraging NCQA Accreditation to promote quality. As they move their high-risk/ high-need aging populations to managed care, their expectations of plans and CBOs have evolved. For Medicaid managed care states, NCQA Health Plan Accreditation is a tool to underscore efficient use of resources, including case management/care coordination for beneficiaries.
Today, 31 managed care states use NCQA Accreditation as a tool to ensure quality; 5 have added LTSS Distinction as a contract requirement to include NCQA’s MLTSS review specifically. Examples of existing state policies for LTSS Accreditation:
- LTSS Distinction in State Medicaid Managed Care Contracts: Kansas, North Carolina, Pennsylvania, Virginia, Tennessee (proposed in California[1] and Arizona[2] plans future contracts).
- LTSS accreditation standards in CBO Requirements:
- Massachusetts Adult Foster Care (multiple accreditors accepted)
- NCQA CM-LTSS proposed in Ohio as a requirement for AAAs.
Comment of Support: A state-designed roadmap with clearly defined expectations for plans and CBO relationships, including collaborating to meet quality standards (accreditation and measure reporting), will yield better alignment and accountability for the system and an improved experience of care for enrollees.
State’s Roles in Supporting Community Integrated Health Networks
We applaud ACL’s focus on Community Integrated Health Networks (CIHN); it is the right direction to ensure that CBOs are primary stakeholders as value-based care models advance.
NCQA has a rich and proven history in managed care and with CBOs. Responding to a demand from our CBO partners for a way to distinguish themselves, NCQA created Case Management for Long- Term Service and Supports Accreditation, which helps CBOs show their readiness for increased accountability to states and managed care organizations. Given that most Medicaid plans are NCQA Accredited, states and organizations are looking for CBOs that have committed to implementing the critical infrastructure needed to deliver high-quality case management for LTSS. Alignment between NCQA LTSS programs provides states the needed oversight of person-centered care coordination of LTSS between plans and CBOs.
Comment of Support: In states using an MLTSS model, create a formal role for CBOs as partners and conduits to the community (p. 20). The CM-LTSS program supports such partnerships by aligning expectations CBOs must meet with expectations health plans must meet as part of state and federal requirements.
Policy Levers to Support Evolution of Aging and Disability Networks
Medicaid Policy Levers:
As states look to optimize relationships with existing networks to address complex medical and social supports needs of older adults and people with disabilities, NCQA continues to be a resource with person-centered solutions that align with state MLTSS and non-MLTSS programs. As noted in the ACL Strategy draft (p. 10) Alabama’s AAAs are using NCQA Accreditation to transform their aging and disability networks. In Massachusetts, the Adult Foster Care program is using Accreditation as a bar for quality in its contracted network. NCQA CM-LTSS Accreditation is also being considered for AAAs in Ohio that serve dual-eligible enrollees.
CBOs, including I/DD providers, in 14 states are seeking NCQA Accreditation independently of state expectations as a means to create needed infrastructure for quality and accountability and to support future expectations for reporting on the services they coordinate and deliver.
Comment of Support: Accreditation of CBOs is a tool for states to support current accountability and ongoing quality improvement efforts of the aging and disability network.
Data Coordination and Alignment
Building IT infrastructure. We support ACL’s work to address the gap in health information technology (IT) infrastructure in the aging and disability network as outlined in the draft Federal Health IT Strategic Plan.[3] As noted by the Strategy’s example of Missouri’s state-based care plan development and care coordination platform, we agree that a robust IT infrastructure is critical to supporting good care and tracking accountability. As states create such infrastructure, factoring in measurement and reporting will be important in driving high-quality care.
With support from The SCAN Foundation through the Long-Term Services and Supports Quality Reporting Learning Collaborative grant, NCQA facilitated a learning collaborative in 2019 that engaged 16 health plans and 2 CBOs across 7 states to report and use the new HEDIS®[4] LTSS measures (see Exhibit A). These measures should be considered as states evaluate their IT infrastructure needs to ensure maximum potential for reporting. Several states, including Pennsylvania and Florida, currently require health plans to report these LTSS measures.
NCQA Recommendation: States should consider requiring reporting of LTSS measures for plans and CBOs as a tool for quality improvement and incentivizing implementation of strong policies and procedures for care coordination.
Section 2: Building State-Driven Roadmaps
Leadership and Policy Opportunities
Improving care coordination. We agree that LTSS Distinction is a tool states can build into contracts for D-SNPs to help them meet enhanced CY21 care coordination requirements. Currently, 26 states have existing NCQA Health Plan Accreditation requirements for Medicaid. Extending the requirements to
D-SNPs, through MIPPA contracts, will align state quality priorities for both Medicare and Medicaid benefits.
Comment of Support – ACL Policy Action Item: “Specifically, state aging, disability, and Medicaid program leaders can collaborate on State Medicaid Agency Contract (SMAC) or MIPPA contract requirements for D-SNPs to clarify how aging and disability networks can satisfy care coordination and Medicare-Medicaid integration requirements that must be implemented in CY 2021.”[5] States can leverage existing care transition standards, such as those in NCQA LTSS programs. Health plan contracts should include language around two-/three-way data sharing and include models for coordinating care across payers.
Data integration: NCQA is actively working with CMS, states, plans and providers to evolve how performance measures are collected and reported. Our 2020 Digital Quality Summit featured presentations from Pennsylvania, Colorado, North Carolina, Oregon and New Jersey on their journeys to build digital measurement infrastructure. Each is leveraging HIEs and engaging or planning for incorporating SDOH data. Presenters and participants shared their interest in validated data and harnessing existing reporting via HIEs, as noted in the Data Coordination and Alignment section of the ACL draft, which highlights work in Oklahoma and Maryland.
The role of community information exchanges (CIE). NCQA remains cautiously optimistic about the new technologies and data sources available to support members with LTSS and SDOH needs; for example, CIEs, which are ecosystems of health care and community partners that share information on the individuals they serve through standardized data collection. Some CIEs may include a resource database and an integrated software platform to coordinate care planning and facilitate bidirectional referrals to patients/members and health care providers. This approach should strengthen partners’ capacity to plan care. At present, quality and accountability for integration of social care is undefined and unmeasured. NCQA is interested in exploring how we might promote quality in a newly emerging data ecosystem.
Comment of Support – ACL Policy Action Item: We support the recommendation to create a data integration plan at a state level that promotes state agency partnership, enables improved data sharing and care coordination and ultimately leads to more effective management of members’ care and use of state resources.
We appreciate the opportunity to comment on ACL’s Strategic Framework for Action for States. We welcome a future conversation on the roles of telehealth, as well as CIEs, in supporting plans and CBOs, and the evolving ways in which measurement can be used to support monitoring and evaluation of the systems delivering care. We look forward to working with ACL and states on implementing the strategy.
Kristine Thurston Toppe, MPH
AVP of State Affairs
National Committee for Quality Assurance
Exhibit A: HEDIS LTSS Measures
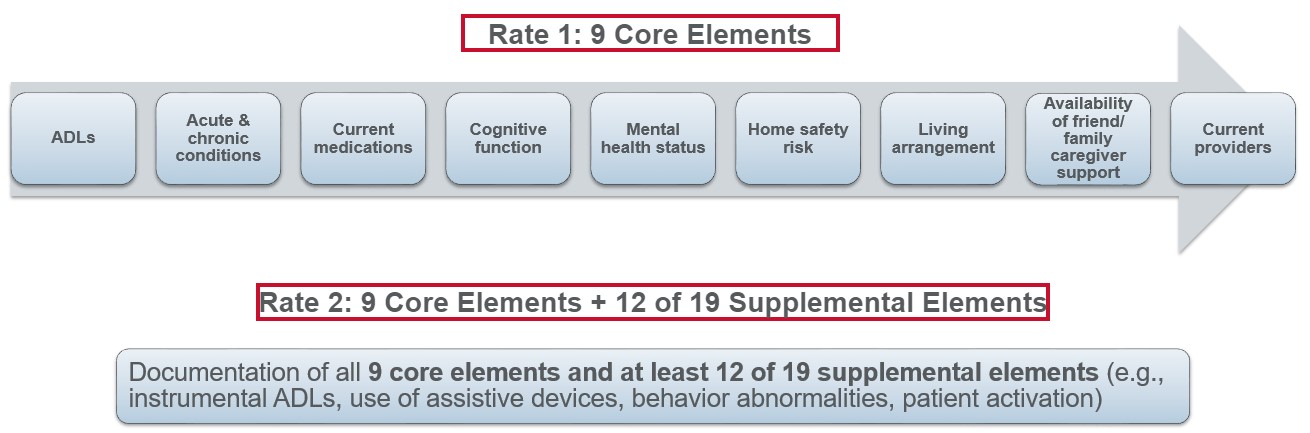
LTSS Comprehensive Assessment and Update (LTSS-CAU)
The percentage of LTSS members 18 years and older who have documentation of an in-home comprehensive assessment annually (for established members) or within 90 days of enrollment (for new members).
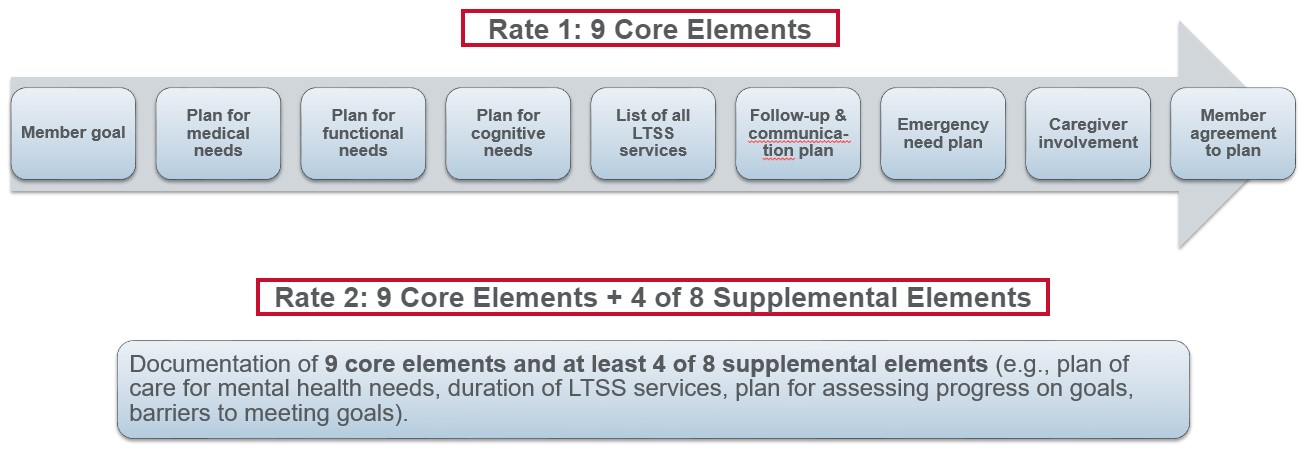
LTSS Comprehensive Care Plan and Update (LTSS-CPU)
The percentage of LTSS members 18 years and older who have documentation of a comprehensive LTSS care plan completed face-to-face annually (for established members) or within 120 days of enrollment (for new members).
LTSS Shared Care Plan with Primary Care Practitioner (LTSS-SCP)
The percentage of LTSS members 18 years and older with a care plan that was transmitted to their primary care practitioner (PCP) or other documented medical care practitioner identified by the enrollee within 30 days of its development.
LTSS Reassessment/Care Plan Update After Inpatient Discharge
(LTSS-RAC)
The percentage of inpatient discharges for LTSS members 18 years and older for whom a reassessment and care plan update occurred within 30 days of discharge.
- Rate 1: Reassessment within 30 days.
- Rate 2: Reassessment and care plan update within 30 days.
| · Measures are reported using data from case management systems for a systematic sample of members. · HEDIS Measurement Year 2020 Specifications are available for download at: http://store.ncqa.org/index.php/catalog/product/view/id/3614/s/hedis-2020-technical-specifications-for-long-term-services-and-supports-measures-epub/ |
[1] https://www.dhcs.ca.gov/provgovpart/Pages/NCQAAccreditation.aspx
[2] https://www.azahcccs.gov/PlansProviders/Downloads/HealthPlans/Jul2020/Contract_Changes.pdf
[3]https://www.healthit.gov/sites/default/files/page/2020-01/2020-2025FederalHealthIT%20StrategicPlan_0.pdf
[4]HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
[5]https://www.integratedcareresourcecenter.com/sites/default/files/ICRC_Medicaid_Enrollment_Service_Use_Info_ 12_2019. pdf
