February 4, 2022
Senate Committee on Health, Education, Labor and Pensions
428 Senate Dirksen Office Building
Washington, DC 20510
Dear Chair Murray and Ranking Member Burr:
The National Committee for Quality Assurance (NCQA) thanks you for the opportunity to respond to the request for stakeholder feedback on the PREVENT Pandemics Act discussion draft. NCQA will comment specifically on Title II—Improving Public Health Preparedness and Response Capacity (Sections 201 and 213).
NCQA is a private, 501(c)(3) not-for-profit organization dedicated to improving health care quality through our Accreditation and measurement programs. We are a national leader in quality oversight and we are at the forefront of the movement to modernize the exchange of health information. Leveraging our strengths as a trusted third party, we work with federal agencies, states, practitioners and managed care organizations to drive alignment, improve quality and advance health equity across the country. With over 30 years of improving the quality of American health care, we offer the following recommendations to the Committee to strengthen the nation’s ability to prepare for and respond to future pandemics.
Sec 201—Addressing Social Determinants of Health and Improving Health Outcomes
The ongoing public health emergency has exacerbated our nation’s health inequities and our ability to capture the magnitude of disparities is hindered by incomplete or missing data. To scale evidence-based solutions to address health inequities and SDOH, we must ensure that HHS has the resources to finance and evaluate innovative models for their impact on health outcomes. We were encouraged by the Committee’s draft proposal to authorize the HHS Secretary to issue grants, contracts and technical assistance to disseminate effective strategies for reducing health disparities and improving health outcomes by addressing SDOH.
Data is crucial to interventions that reduce health inequities and improve individual and population health outcomes. We recommend the Committee stipulate that grantees and contractors must collect, and report to HHS, demographic and SDOH data, consistent with national standards for data exchange such as USCDI.
Additionally, we recommend that the Committee encourage HHS to study how national accreditation standards can enhance organizations’ capacity to address SDOH and disseminate best practices to advance health equity. Since the pandemic began, policymakers have turned to NCQA’s Health Equity Accreditation to establish requirements that can close inequitable gaps in health outcomes. Health Equity Accreditation is not a new program; rather, we rebranded and updated our Multicultural Health Care Distinction program, which has been a framework for health care organizations to close inequitable health outcomes for over a decade. That program was designed after the HHS Office of Minority Health’s CLAS Standards.
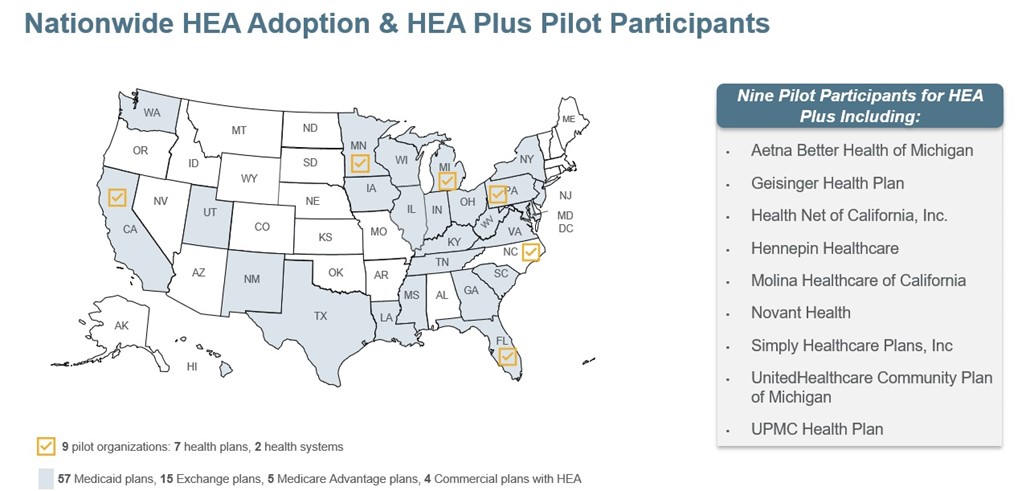
In November 2021, with assistance from nine leading health organizations across the country, we launched a pilot program to develop Health Equity Accreditation Plus. This program helps health care organizations establish processes and cross-sector partnerships that identify and address social risk factors and social needs of the people in their communities. NCQA is working with pilot participants to test the concepts and application of this new program. Feedback will help us enhance and streamline its standards. Health Equity Accreditation Plus will be available to health plans, health systems and other care organizations this spring.
Sec 213—Supporting Public Health Data Availability and Access
NCQA was pleased to see the proposed amendments to improve public health data standards for electronic health information exchange for case reporting, syndromic surveillance, vital statistics and laboratory reporting. We encourage the Committee to add quality measure reporting to Sec 213 (B) Selection of Data and Technology Standards.
As the Committee deliberates on enhancements to the public health infrastructure for future pandemics, it will be essential to include the components of a fully interoperable health system. The nation needs an infrastructure that allows rapid dissemination of new knowledge based on trustworthy data. The COVID-19 pandemic highlighted our public health system’s inability to rapidly develop clinical guidelines, related decision supports and quality measures to assess their implementation.
For more than 30 years, quality measurement has driven remarkable improvements in health care—but the current quality measurement system is fragmented, labor-intensive, inconsistent and retrospective. Clinical quality measurement has provided an effective use case for efforts targeted at improving the quality and accessibility of data produced by health care entities (i.e., laboratories), but these efforts have not typically included the use of public health information. Digital Quality Measures (dQMs) specified using interoperability standards offer a unique opportunity to expand the use of high-quality, standardized information from across the clinical and public health data spectrums, further promoting their use.
Improving the accuracy and availability of comprehensive health care information can result in better measures, better measurement systems and better response to future pandemics. It is important to recognize the role of ongoing efforts to incorporate public health information into clinical measurement systems (e.g., the CDC’s MedMorph project), which can support not only quality, but also the nation’s ability to respond to public health emergencies.
dQMs are a critical component of a fully interoperable learning heath system that generates accurate and reliable knowledge at a time when it is most useful. The Committee has the opportunity to encourage HHS to accelerate the move to a fully digital quality ecosystem with dQMs as a core component. CMS has already started to explore the transition to all dQMs by releasing an RFI in the 2022 Medicare Hospital Inpatient Prospective Payment System and Long Term Care Hospital proposed rule.
We remain committed to improving the nation’s health care system and we welcome a discussion on our recommendations. Thank you again for the opportunity to comment. We appreciate the Senate HELP Committee’s efforts to build a stronger public health preparedness and response system. If you have any questions, please contact Eric Musser, NCQA Director of Federal Affairs, at (202) 955-3590 or at musser@ncqa.org.
Sincerely,
Margaret E. O’Kane
President
