January 27, 2022
Chiquita Brooks-LaSure, Administrator
Centers for Medicare & Medicaid Services
7500 Security Blvd.
Baltimore MD 21244
Attention: CMS-9911-P
Dear Administrator Brooks-LaSure:
Thank you for the opportunity to comment on the 2023 Notice of Proposed Benefit and Payment Parameters for Qualified Health Plans (QHP). The National Committee for Quality Assurance (NCQA) will comment specifically on the requested feedback and proposals for advancing health equity. NCQA is an independent, not-for-profit organization dedicated to improving health care quality and reducing health inequities through measurement, transparency and accountability.
Although health disparities in the American health care system have been long researched and documented, there has been no coordinated national effort to rectify them and drive accountability across the system. With this administration’s leadership and in collaboration with trusted partners, we must now define the role of health care organizations in advancing health equity. We appreciate CMS’s consideration and offer the following comments.
- CMS seeks input on requiring QHP issuers to obtain the National Committee for Quality Assurance (NCQA) Health Equity Accreditation in addition to their existing accreditation requirements
Health Equity Accreditation: We were pleased to see CMS’s request for feedback on requiring QHPs to achieve NCQA Health Equity Accreditation. NCQA commends CMS’s commitment to health equity throughout the agency and is encouraged by the administration’s proposed rules to ensure that organizations supporting federal programs meet the highest bar for quality and equitable outcomes. We believe accreditation can be a primary lever to advance health equity and create the necessary data collection and quality improvement processes to measure, report and improve on outcomes based on race, ethnicity, sexual orientation, gender identity, disability and other aspects.
NCQA is committed to being an inclusive, equity-focused organization and therefore recognizes the challenges other organizations will encounter as part of the Health Equity Accreditation process. The process provides flexibility for organizations at differing starting points along the continuum of growing into equity-focused organizations.
Guided by expertise and lived experience, Health Equity Accreditation is based on the pursuit of equity. For example, because addressing systemic injustices that perpetuate inequities begins with structural changes in organizations, we have included structural assessment and improvements in program requirements. Our Health Equity Accreditation standards provide a supportive glidepath to organizations becoming equity focused over time and at a reasonable pace.
Health Equity Accreditation is not a new program; rather, we have rebranded and updated our Multicultural Health Care Distinction program, which has been a framework for health care organizations to close inequitable health outcomes for over a decade. The program was designed after the HHS Office of Minority Health’s Culturally and Linguistically Appropriate Services (CLAS) Standards.
Health Equity Accreditation comprises six foundational standard categories, tightly linked with CLAS, on which health care organizations are surveyed and scored:
- Organizational Readiness. The organization is committed to health equity by building a diverse and inclusive staff.
- Race, Ethnicity, Language, Gender Identity and Sexual Orientation Data. The organization gathers data on race, ethnicity, language, gender identity and sexual orientation using standardized methods.
- Access and Availability of Language Services. To effectively communicate with patients, organizations provide materials and services in the languages patients use and understand.
- Practitioner Network Cultural Responsiveness. The organization’s practitioner network is capable of serving its diverse membership and is responsive to member needs and preferences.
- Cultural and Linguistically Appropriate Services. The organization continually improves its services to meet the needs of multicultural populations.
- Reducing Health Care Disparities. The organization uses data on race, ethnicity, language, gender identity and sexual orientation to assess the existence of disparities and focus on improving provision of CLAS and decreasing health care disparities.
Since the original program’s release in 2010, Accreditation has been achieved by 75 organizations across the country and continues to garner exceptional interest from state and federal policymakers. In the last 3 years, five state Medicaid programs have required the program in managed care contracts, and both the California and Washington, DC, QHP Exchanges have required Health Equity Accreditation for all issuers.
NCQA strongly supports requiring Health Equity Accreditation for QHP issuers, but feels CMS should give issuers ample notice to meet requirements.
Health Equity Accreditation Plus: Enthusiasm for Health Equity Accreditation energized us to do more. In November 2021, with assistance from nine leading health organizations across the country, we launched a pilot program to develop Health Equity Accreditation Plus. This program helps health care organizations establish processes and cross-sector partnerships that identify and address social risk factors and social needs of the people in their communities. NCQA is working with pilot participants to test the concepts and application of this new program. Feedback will help us further review, enhance and
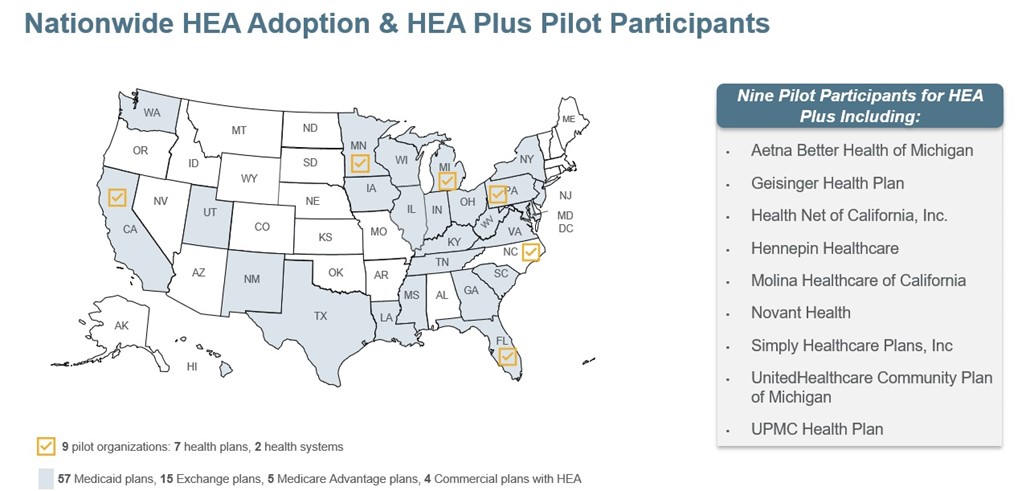
streamline its standards. Health Equity Accreditation Plus will be available to health plans, health systems and other care organizations this spring.
- Update quality improvement strategy standards to require issuers to address health and health care disparities
We support CMS’s proposal to require QHP issuers to address reduction of health and health care disparities in QIS submissions. The QIS requirement for QHPs is another avenue for CMS to drive accountability for advancing health equity. NCQA Health Equity Accredited QHPs will have quality improvement processes in place to close inequitable gaps in health outcomes and succeed on the QIS requirement.
- Prohibit discrimination based on sexual orientation and gender identity
We applaud CMS’s proposal to prohibit Exchanges, issuers, agents and brokers from discriminating against consumers based on sexual orientation and gender identity. The previous administration was misguided in revising CMS regulations and removing nondiscrimination protections for gender identity and sexual orientation in the 2020 HHS final rule on Section 1557. We agree with the current administration that without protection from discrimination, LGBTQI+ individuals may continue to face barriers to accessing medically necessary health care.
Thank you for the opportunity to comment. We remain committed to working with CMS to build a more equitable, sustainable and responsible American health care system. We welcome a discussion on our experience and recommendation to require QHPs to obtain NCQA’s Health Equity Accreditation. If you have any questions, please contact Eric Musser, Director of Federal Affairs, at (202) 955-3590 or at musser@ncqa.org.
Sincerely,
Margaret E. O’Kane
President
