January 5, 2021
Seema Verma, Administrator
Centers for Medicare & Medicaid Services
7500 Security Blvd.
Baltimore MD 61244
Attention: CMS-9123-P
Dear Administrator Verma:
Thank you for the opportunity to comment on the proposed rule to improve prior authorization and data exchange in Medicaid, the Children’s Health Insurance Program (CHIP) and Qualified Health Plans (QHPs). The National Committee for Quality Assurance (NCQA) supports proposals to improve electronic data sharing and prior authorization, as there is an urgent need for both to reduce burden and improve the ability to measure and improve quality. We also believe it is critical to establish standards for electronic exchange of social risk data to reduce disparities and promote health equity. We support both the Gravity Project’s approach to doing this as well as development of additional Z codes. We provide detailed comments on these and other issues in the proposed rule below.
Electronic Data Sharing: We support proposals to improve Medicaid, CHIP and QHP electronic data sharing by:
- Requiring implementation of the Payer-to-Payer API to support exchange of patient data, U.S. Core Data for Interoperability (USCDI) clinical data, and information related to pending and active prior authorization decisions.
- Requiring exchange of data with patients, as in 21st Century Cures Act rules for other programs, so patients can maintain an electronic copy of their health information, share data directly with their providers, and bring their health information with them as they move from one payer to another.
Ensuring that data flows to and with patients as they move from one plan to another will improve our ability to measure quality, as many quality measures have lookback periods of one and sometimes several years and now exclude patients not in one plan for at least 12 months. Data flow also facilitates NCQA and CMS shared goal of moving to digital quality measures (dQM) that use data generated in the normal course of care and kept in electronic health records (EHRs), registries, health information exchanges (HIE) and other electronic sources. Deriving quality measurement data from electronic sources can reduce reporting burden, improve the accuracy of results, and support measures that are more meaningful than traditional reporting based on claims data.
In response to your related request for information, these same policies should apply to Medicare Advantage plans and we encourage you to extend them in future rule making for that program.
Regarding your request for information on how to facilitate electronic data exchange between and with behavioral health care providers and community-based organizations, we encourage you to use the same approach as for other settings of care with APIs to the extent feasible. Establishing a uniform approach for all settings will minimize burden and ensure consistency across payers and programs.
Prior Authorization: We also support the proposals to improve prior authorization by:
- Requiring application program interfaces (API) to let providers know in advance what documentation they need in prior authorization requests for each payer, and to facilitate prior authorization requests and responses electronically within providers’ existing workflow to eliminate the need for calls and faxes;
- Reducing the maximum time to approve prior authorization requests to 72 hours for urgent & seven calendar days for non-urgent requests and requiring payers to provide a specific reason for denials.
- Requiring payers to report metrics on how many procedures they authorize or deny.
We also support the concept of “Gold Carding” programs in quality Star Ratings and prior authorization programs. This is a common-sense approach to recognizing and reducing burden on high-performing clinicians who consistently request authorization for appropriate services. We believe Patient-Centered Medical Home (PCMH) and Patient-Centered Specialty Practice recognition can be an additional factor to complement Gold Card programs. Clinicians in NCQA PCMHs and PCSPs meet rigorous standards for following evidence-based standards of care—that align with the goals of prior authorization requirements. They also meet similar standards for expanded access, population health, quality improvement and are well-documented to improve quality and reduce avoidable utilization.
Current prior authorization policies suffer from many of the same challenges as quality measures that we are working to address by moving to digital quality measures (dQM). They are based on administrative data and guidelines and there is a broad desire to align them more closely with clinical best practices and treatment guidelines. They also are similar to payer-driven quality and value-based payment programs in that they are a huge source of administrative burden on providers, interrupt physician workflows and negatively impact patient experience.
The same arguments, approaches and standards for clinical reasoning and data collection for dQM can and should apply to digitizing prior authorization. Common approaches across plans and products, common mechanisms for sharing and validating data, and common infrastructure for running authorization guideline logic at the point of care make sense. Establishing common tools, infrastructure, standards, and implementation in this way is an important step to relieve prior authorization burden and allow for quicker response time decisions on prior authorization from payers to better meet patient needs.
Standards for Social Risk Data: Regarding your request for information on standards for electronic exchange of social risk data, NCQA believes this is an essential priority for efforts to address social determinants of health (SDOH), reduce disparities and promote health equity. High quality care equals equitable care, and inequitable care is low quality care.
SDOH influence up to 80% of health status at a population level, yet there is still no consistent way to document and communicate these factors in electronic data exchange. Setting such standards is a necessary step in ensuring that our health system is enabled, fully resourced, and effectively engaged in promoting health equity and holding stakeholders accountable for doing so.
We support the work of The Gravity Project, a nationwide multi-stakeholder collaborative, to build consensus data elements, standards, and specifications for SDOH data capture, exchange, use, and aggregation. Gravity Project this year submitted a new SDOH data class to the Office of the National Coordinator for Health IT (ONC). ONC has categorized The Gravity Project’s submission as Level 2. This indicates that ONC agrees the SDOH data elements demonstrate extensive existing use and exchange between health systems, that use cases show significant value to current and potential users and to nationwide interoperability, and that any burdens or challenges would be reasonable to overcome relative to the overall impact of the data elements. We have encouraged ONC to include Gravity Project’s approach to adding structured SDOH data to the U.S. Core Data for Interoperability (USCDI) so it can be in the draft version 2 up for public comment next month.
We also support expanding ICD-10 Z codes for SDOH, as suggested by The Gravity Project. These codes are an important contribution to our ability to assess quality of care and promote health equity. Establishing more comprehensive Z codes can further increase standardization in SDOH data collection and help in tracking quality and outcomes with measure stratification for patients with and without certain SDOH factors.
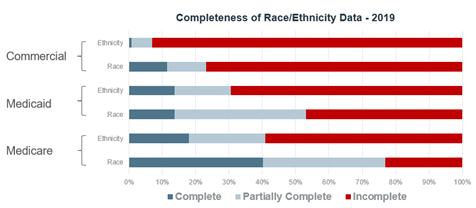 Closely related to the need for SDOH data standards is the need for better racial, ethnic and language composition data, which is also essential for effectively addressing health equity and SDOH. Collection of such data among health plans varies substantially by product line. Most Medicaid and commercial health plans do not consistently collect or report race or ethnicity data on their membership. However, in Medicare Advantage 40% of plans have complete data on over 95% of their members and nearly another 40% have it on over 50% of their members. This demonstrates that we can obtain these data, which, along with other SDOH data, we need to stratify quality measures to rate and compare inequities between subgroups, and to create and adapt measures of equity and outcomes.
Closely related to the need for SDOH data standards is the need for better racial, ethnic and language composition data, which is also essential for effectively addressing health equity and SDOH. Collection of such data among health plans varies substantially by product line. Most Medicaid and commercial health plans do not consistently collect or report race or ethnicity data on their membership. However, in Medicare Advantage 40% of plans have complete data on over 95% of their members and nearly another 40% have it on over 50% of their members. This demonstrates that we can obtain these data, which, along with other SDOH data, we need to stratify quality measures to rate and compare inequities between subgroups, and to create and adapt measures of equity and outcomes.
NCQA is committed to helping health plans and the nation address SDOH, as reflected in our recently released Social Determinants of Health Resource Guide, a reference for designing and implementing strategies to address SDOH for commercial populations.
We are committed to improving data standards and better race, ethnicity and language data will be essential for strengthening our ability to do so. We also are working to develop best practices for collection of race, ethnicity and language data and to explore how we can assess equity in more areas and in new ways.
Thank you again for the opportunity comment on the proposed rule. If you have any questions, please contact Paul Cotton, Director of Federal Affairs, at (202) 955-5162 or cotton@ncqa.org.
Sincerely,
Margaret E. O’Kane
President
