March 6, 2015
Sean Cavanaugh, Deputy Administrator
Centers for Medicare and Medicaid Services
Director, Center for Medicare
AdvanceNotice2016@cms.hhs.gov
Dear Mr. Cavanaugh:
Thank you for the opportunity to comment on the Advance Notice of Methodological Changes for Calendar Year 2016 for Medicare Advantage Call Letter. We support many of your proposals, but are concerned that reduced weighting for some measures where performance is most associated with plan enrollee’s socioeconomic status may have unintended consequences.
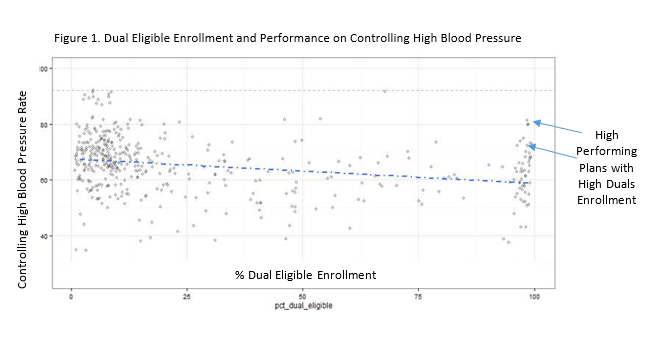
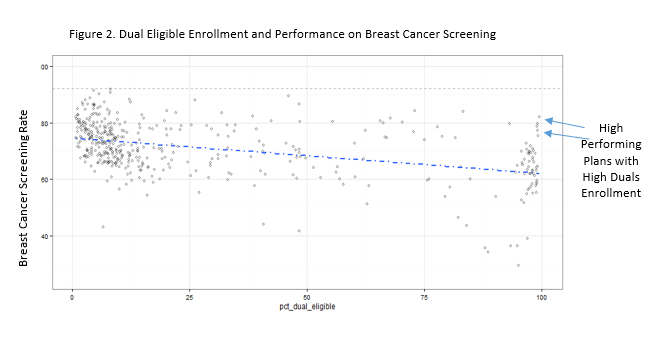
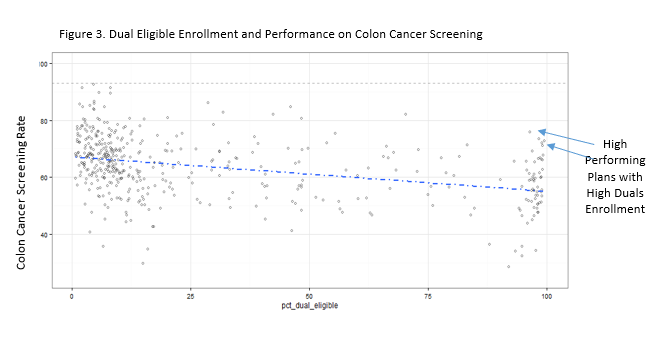
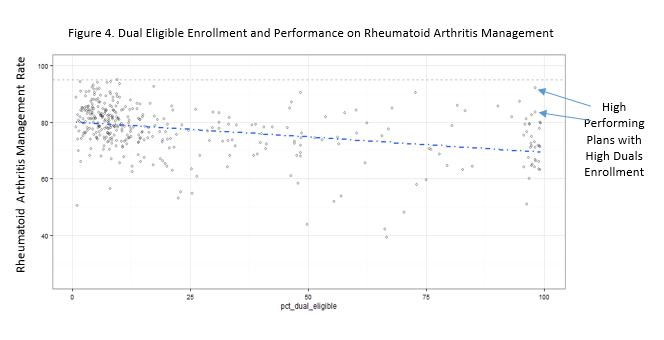
Risk Adjustment: We greatly appreciate your reference to our concerns that socioeconomic risk adjustment masks disparities, and that we should instead make sure plans and providers have resources and skills to reduce disparities. We also appreciate that some plans serving large low income populations – with notable exceptions – do worse on some measures, decreasing their ability to earn bonuses that could help them to improve. We understand your interest in balancing these competing concerns by reducing weights temporarily for measures where results are most associated with socioeconomic status.1
However, it is important to note that this association does not prove causation. Many plans with large low income populations do well above average on some measures for which you propose reduced weighting (see Appendix 1). High performance among these plans is explained by a growing body of evidence that high performance can be achieved, regardless of patient income, through person-centered care provided in Patient-Centered Medical Homes.2 This specifically includes performance on the breast and colorectal cancer screening measures you propose for down weighting.3 Socioeconomic disparities in mortality rates are particularly acute for these cancers.4,5
In fact, the association between socioeconomics and performance may be an artifact of less patient-centered care and patient activation. It is important that plans strive to address any poor performance rates, rather than dismiss them as something that cannot be helped.
Reduced weighting would minimize rewards for high performance earned among plans serving large dual eligible populations by providing this type of patient-centered care. It also would diminish focus on the important clinical issues these measures address. Maintaining a strong focus and rewards for good performance is especially important for colorectal cancer screening, which is a powerful tool for preventing avoidable death and more costly care.6 If implemented at all, reduced weighting must be a very temporary step toward much more thoughtful approaches. We are committed to working with you and other colleagues to ensure both accurate measurement and fair payment while striving to eliminate disparities.
Other Star Ratings Changes: We support eliminating all pre-determined four-Star thresholds, as there is consistently more improvement on measures with no pre-set target. We support addition of the Medication Therapy Management Completion measure and other measure adjustments to align with HEDIS®7 changes. We support wider use of independent data validation to ensure accuracy and thus fairness to all plans, which is particularly important under pay-for-performance. We also support termination of plans with less than three stars for three consecutive years, as proposed. As for developing a separate Stars Rating system for integrated Medicare and Medicaid plans, we are working to develop measures and accreditation for such plans caring for people with complex needs. We would be happy to update you on this ongoing work, which may help inform your thoughts.
Provider Directory Accuracy: We appreciate your provider directory inaccuracy concerns and are exploring ways to further address this in our health plan accreditation program as well. We found, however, that the suggestion to require plans to frequently contact each provider office to re-verify information would require significant expenditures that likely would be passed onto consumers. We also learned that requiring plans to merely send a notice to practices asking them to reply if the plan’s current information on them is no longer accurate would not yield significant responses to improve directory accuracy. We therefore are now exploring a less costly option of requiring plans to re-verify information on a representative sample of their networks and take any needed actions to improve.
Drug Coverage Denials: We support adding a section to drug coverage denial notices for listing specific information plans need to provide coverage. We require this now for plans that we accredit, and believe it should be required for all appeals, both Part D drug appeals and Part C appeals as well.
Thank you again for the opportunity to comment on the draft call letter. If you have questions, please contact our Director of Federal Affairs, Paul Cotton, at cotton@ncqa.org or (202) 955 5162.
Sincerely,
Margaret E. O’Kane
President
Appendix 1 –Performance on Measures Proposed for Reduced Weighting
The scatter plot in Figure 1 shows that some plans with high levels of dual eligible enrollment perform well above average on the “Controlling High Blood Pressure” HEDIS measure.
The scatter plot in Figure 2 shows that some plans with high levels of dual eligible enrollment perform well above average on the “Breast Cancer Screening” HEDIS measure.
The scatter plot in Figure 3 shows that some plans with high levels of dual eligible enrollment perform well above average on the “Colon Cancer Screening” HEDIS measure.
The scatter plot in Figure 4 shows that some plans with high levels of dual eligible enrollment perform well above average on the “Rheumatoid Arthritis Management” HEDIS measure.
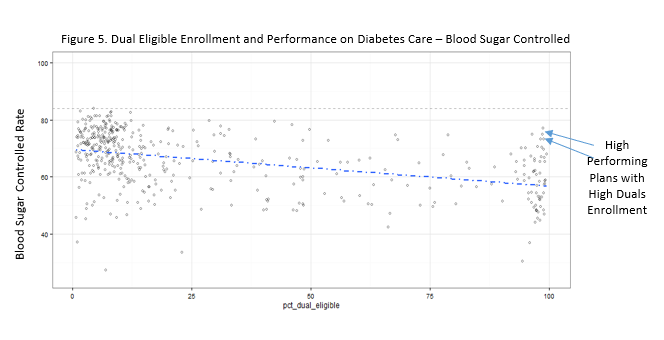
The scatter plot in Figure 5 shows that some plans with high levels of dual eligible enrollment perform well above average on the “Diabetes Care – Blood Sugar Controlled” HEDIS measure.
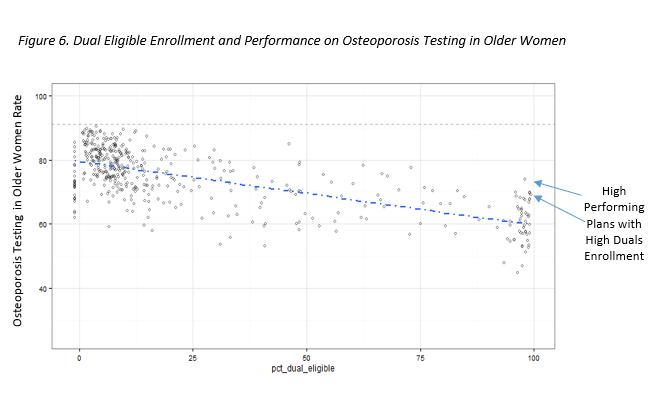
The scatter plot in Figure 6 shows that some plans with high levels of dual eligible enrollment perform well above average on the HEDIS measure on Osteoporosis Testing in Older Women
- Breast Cancer Screening, Colorectal Cancer Screening, Osteoporosis Management in Women who had a Fracture, Rheumatoid Arthritis Management, Reducing the Risk of Falling, Diabetes Care – Blood Sugar Controlled, and Medication Adherence for Hypertension [RAS antagonists]
- Berenson, J et al, Achieving Better Quality of Care for Low-Income Populations: The Role of Health Insurance and the Medical Home for Reducing Health Inequities, Commonwealth Fund, May 2012.
- Markovitz, A. et al, Patient-Centered Medical Home Implementation and Use of Preventive Services, The Role of Practice Socioeconomic Context, JAMA Internal Medicine, February, 2015.
- Hershman, Disparities in Breast Cancer Care Linked to Net Worth, Journal of Clinical Oncology, February, 2015.
- American Cancer Society, Half of Premature Colon Cancer Deaths Linked to Disparities, November, 2014
- United States Preventive Services Task Force, Colorectal Cancer Screening Recommendations, October 2008.
- HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
