Disrupting Disparities With Data—And a Focus on Community
October 14, 2025 · NCQA Communications
The conversation continues at the Health Innovation Summit with an inspiring keynote session on reducing health disparities. Moderator Tamara Thomas of Aledade joined Donald Erwin and Alexandria Johnson of St. Thomas Community Health Center and Danielle Brooks of AmeriHealth Caritas to discuss practical, data-driven approaches to reducing health disparities.
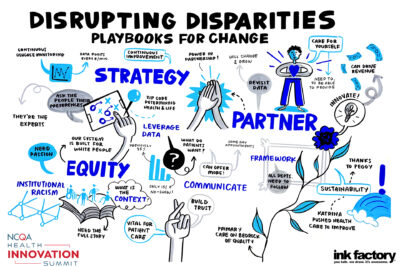
“Our session is called Disrupting Disparities: Playbooks for Change. But we’re not talking about football plays—we’re talking about saving lives and doing so inclusively,” says Thomas. “When we think about the importance of these playbooks, it is much like football. You need to have a strategy, you need to have teamwork and sometimes you need to have the courage to call a different play when the old ones aren’t working. And today in health care, we need some new plays.”
How Collecting Data Helped Uncover Patient Needs
St. Thomas Community Health Center is a federally qualified health center (FQHC) in New Orleans that serves more than 22,000 patients each year across seven clinics. It has also earned NCQA’s Patient-Centered Medical Home Recognition.
Reducing No-Show Rates
In 2021, the no-show rate for appointments at St. Thomas was 35%. The team tried emails, text reminders and phone calls to patients, but nothing seemed to make a difference. They decided to start collecting data to understand what patients really wanted. Every time a patient requested an appointment, the staff noted the date they wanted to be seen, the practitioner they wanted to see and the type of appointment.
When they looked at the data, they identified a significant gap: 40% of patients wanted same-day care and 22% wanted next-day care, but St. Thomas had 3-4 week wait times for primary care appointments. The team made a drastic change to their scheduling practice to accommodate same-day and next-day care and the no-show rate decreased from 35% to 15%.
Improving Clinic Wait Times
Next, the team decided to tackle wait times in the clinics. “For our patient population, it’s crucial that we run on time because they have to get back to work or they have to get back to their children,” says Johnson. “When our clinic runs late, we force our patients to choose between getting the medical care they need or making sure they keep their job or meet their kids’ needs.”
Once again, the team at St. Thomas looked at the data: How long patients sat in the waiting room, how long it took to triage them, how long the patients waited to see the provider. And they found opportunities to improve at every step along the way. For example, they found that patients spent an average of 19 minutes with a practitioner, but appointments were only scheduled for 15 minutes. By extending scheduled appointment times to 20 minutes, they were able to improve timeliness.
“Patients are the experts in their own health care. If you listen to their voices clearly enough, you’re going to get a healthy dose of humility because they know what they’re talking about,” says Erwin. “They’ve told us a hundred times: ‘Stop trying to think for us.’ ‘Stop trying to think about what we want, or what we should want.’ So, we’re listening. And we still work every day to earn the trust of the folks in our community.”
The Power of Partnerships
Too often, health care operates in silos. Having opportunities to partner with industry stakeholders and the community can provide context to see if the solutions we are developing will actually work. Brooks shared her experience participating in NCQA’s Perinatal Health Measurement Advisory Panel, which gathered a wide range of perspectives—payers, care delivery organizations, patients, doulas, advocates—to focus on developing perinatal health measures from a perspective of lived experience.
“Data is wonderful, but data is imperfect and there can be bias in data,” says Brooks. “I can look at as much data as I want, but I also need that context and quantitative learning that comes from listening to the stories of the people in the room.”
Brooks also stressed the importance of viewing health care policy in a historical context. “These disparities are real. We can choose to act on them now, or they’ll get worse over time,” says Brooks. “What may be the policy today, may not be tomorrow. We need to continue to focus on communities, to take solace and learn from those that have gone before us.”
Donald Erwin Receives NCQA’s Health Quality Award
 NCQA’s Founder and President, Peggy O’Kane made a surprise appearance at the end of the keynote session to present Erwin with the Health Quality Award. O’Kane first met Erwin when she visited New Orleans in the aftermath of Hurricane Katrina. The two worked closely together in the years that followed, helping to increase the number of FQHCs and patient-centered medical homes in Louisiana, and improving access to care for uninsured and under-insured people.
NCQA’s Founder and President, Peggy O’Kane made a surprise appearance at the end of the keynote session to present Erwin with the Health Quality Award. O’Kane first met Erwin when she visited New Orleans in the aftermath of Hurricane Katrina. The two worked closely together in the years that followed, helping to increase the number of FQHCs and patient-centered medical homes in Louisiana, and improving access to care for uninsured and under-insured people.
“My visits to St. Thomas were among the most moving experiences I’ve had in my career,” says O’Kane. “Donald Erwin is a true servant leader. He has dedicated his career to the pursuit of high-quality care for all—especially those who are too often left behind due to barriers in access, health status or lived experience. His tireless work, collaborative spirit and visionary leadership have improved countless lives. I am privileged to recognize him and his team’s work.”
Join Us Next Year
Mark your calendar for the 2026 Health Innovation Summit, October 4-7, in Atlanta, Georgia!