A Tribute to National Developmental Disabilities Awareness Month
March 22, 2022 · Paige Cooke
What better time to launch NCQA’s first quarterly LTSS Limelight Series of 2022, than during National Development Disabilities Awareness Month. By the time you finish reading this, you will hopefully have a better understanding of the intellectual/developmentally disabled population, some of the key challenges they face in Medicaid, and how one state has been successfully championing efforts to improve the lives of these incredible members of our society through leveraging telehealth.
National Developmental Disabilities Awareness Month was established by President Reagan in to shine a spotlight on the needs of persons with developmental disabilities and highlight the opportunities available to help them live their lives to the fullest.
Developmental disabilities are defined by the CDC as a group of conditions due to an impairment in physical, learning, language, or behavior areas that begin during the developmental period that may impact day-to-day functioning, and usually last a person’s lifetime. Current estimates show that one in six children between 3 and 17 have one or more disabilities and include diagnoses such as:
- Learning or intellectual disabilities (such as dyslexia or dysgraphia)
- Cerebral palsy
- Autism spectrum disorders (such as Down Syndrome)
- Attention-deficit/hyperactivity disorder (ADD/ADHD)
- Hearing loss
- Vision impairment
- Other developmental delays
Overcoming the Barriers

In the previous LTSS Limelight blog focused on where States were focusing their ARPA funding to advance HCBS programs, we highlighted the increased focus on supporting individuals with intellectual/developmental disabilities (I/DD). Intellectual disability is characterized by significant limitations both in intellectual functioning (reasoning, learning, problem solving) and in adaptive behavior, which covers a range of everyday social and practical skills areas.
As you might imagine, individuals with intellectual/developmental disabilities often require considerable physical, behavioral, and social supports to experience the quality of life they deserve. When born into or faced with additional socio-economic barriers, this can be even more challenging. Unfortunately, the web of coordination is a bit tangled to say the least.
According to the American Association on Intellectual and Development Disabilities (AAIDD) there have been significant barriers in Medicaid, including funding, institutional bias, an increase in crisis of unmet need and a worsening workforce crisis that has only been worsened by the pandemic. AAID and other national organizations/advocacy groups have been hard at work to overcome the barriers state Medicaid agencies have struggled to address, including:
- A patchwork of systems, supports that are often uncoordinated.
- Uncompensated caregivers and the challenge of the high number of retirement age caregivers.
- Individuals w/ IDD not given the authority to make choices and control over funding.
- A funding model that requires members and families to impoverish themselves or remain poor for life.
- Long wait lists for access to services with little guidance and support in the interim.
- Limited availability of affordable housing programs and other needed support services.
Recent Reports
In a recent California Health Care Foundation Report Understanding What Works: Measuring and Monitoring Quality in Medi-Cal’s Home and Community-Based Services, it explains how “the constellation of service needs for people with intellectual and developmental disabilities may influence how care is coordinated, how consumers manage self-direction of their care, the extent to which they involve their family caregivers (and whether HCBS supports are provided to their caregivers), and the number of state agencies that oversee the set of HCBS provided.” This complex reality in coordination of services is not limited to the management of services for I/DD populations in California.
However, there is one state that has taken a truly innovative approach to advance the coordination of services for this important population by leveraging a specialized telehealth program and demonstrated weaving it together on a seamless platform shared between providers, case managers and the state system all captured through a state Health Information Exchange (HIE). (Talk about a Value-Based Payment model win!)
An LTSS Spotlight on Missouri
Earlier this month, I had the pleasure of speaking with Jessica Bax, Director of Missouri’s Division for Developmental Disabilities, a division of the state’s Department of Mental Health. The results of the Division’s partnership with StationMD, that started with a 15,000-member collaboration leveraging a delivery system grant is incredible to say the least!
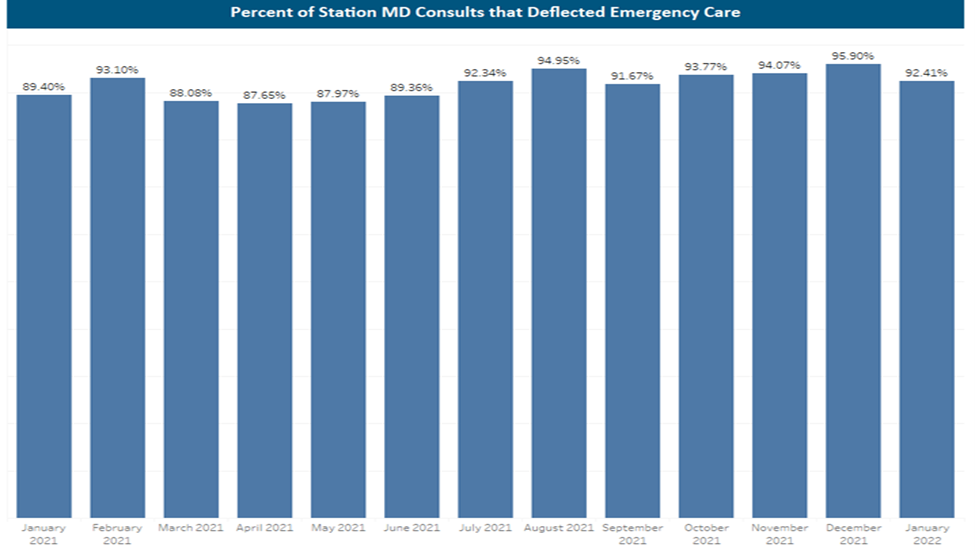
Imagine a 24/7 service providing access to I/DD trained clinicians that can alert emergency rooms of I/DD waiver recipients headed their way to help the providers in the ED(Emergency Department) better serve them when they arrive. Envision a system of support that reduces the stress for family caregivers and paid direct support staff, and empowers clinicians not trained to assist populations with I/DD and access to information about the individual and their specific needs. Well, not only was this made possible through the Division’s work with StationMD, but ALL Medicaid Waiver recipients could use StationMD’s services immediately for ANY medical concerns as of March 2020. The outcomes were 80% in avoided ED visits and 90% of calls are to train employees. Prior to the program, 34-45% off all ED visits results in unjustified admissions or expanded stays in SNFs.
Per Bax, the state advocated for the use of the state’s existing telehealth services well before COVID. However, there was limited success in leveraging these telehealth options for this population because the telehealth doctor was generally not familiar with the population’s specific needs and challenges, and would serve as their irregular primary care physician. When COVID hit, the Division did not want members to access the hospital or urgent care settings unless absolutely necessary to avoid to avoid COVID exposure. Using Cares Act dollars, they set up connections with Station MD who had trained doctors in DD that were aware of the needs of the population and coordinated with members’ primary care physicians, providers, caregivers, and the ED. StationMD allows both paid and unpaid caregivers, as well as Waiver recipients to call and receive assistance regarding medical concerns; Station MD provides consultation and assessment to help determine the best care for the situation. If an ED visit was determined as necessary through consultation, the result of calling EDs in advance reduced wait times and resulted in fewer unnecessary hospital admissions. This was a critical need as ED docs aren’t typically trained to manage the needs of this special population and can be more inclined to administer additional testing due to communication barriers and ultimately admit, said Bax. All of this can be highly disruptive for individuals with IDD, and potentially lead to an overall decline in progress and/or increased behaviors.
Missouri’s Plan
In devising the state’s waiver service, the state worked closely with partners at the National Association of State Directors of Developmental Disabilities Services (NASDDDS)and helped define the service supporting the ability to frame it as a telehealth consultation service. This helped ensure it was made available to every single waiver client. Once that was done, StationMD was positioned to partner with Missouri to build the path towards eLTSS data standards into the case management system to flow into the HIE. Utilizing HCBS enhanced FMAP funding, the state is partnering to build the connections to ensure StationMD has real time access to the care plan, history, case notes and most recent information for every waiver recipient. StationMD also sends data back to the state/Division, care provider and primary care physician, effectively closing the loop of care needed for that individual.
To learn more about this successful state partnership program for I/DD waiver recipients please visit the Missouri Department of Mental Health or StationMDs website to learn more.